I’m Married to an Emergency Room Doctor in New York City
How fighting the pandemic has changed our lives forever
June 9, 2020 · Updated January 31, 2026
“Okay, I’m ready,” Alex says. My husband is wearing his green scrubs under a hospital-issued jacket with his name embroidered on the upper left side, over his heart: Dr. Alexander Fortenko, Emergency Medicine. My eyes catch on the red pressure ulcer that’s been slowly growing on the bridge of his nose.
He looks at me expectantly. He’s waiting for me to recite the incantation I do before each shift. “I love you,” I say. “Be safe. Stay away from sick people.” It’s our talisman — an impossible ask that I hope, against all rationality, will keep him safe. It worries me that he’s come to rely on it.
“I promise I will.” He blows me a kiss and is gone.
. . .
I walk into the hospital and head straight for the doctor’s offices and lockers. I sanitize my hands once I’ve opened the door, and then I take my goggles out of my backpack. These are reusable, and we only get one pair — typically, I clean and resanitize these every few patients, about five or six times in a twelve-hour shift. Then, I put my backpack away into my locker. I make sure I don’t touch anything else except what I absolutely must. While I’m still wearing a surgical mask — the same one I’ve worn from home — I walk into the ER.
The first thing I do is grab an n95 mask from the clerk, who usually keeps track of how many each person has gotten throughout the day. During the peak in New York a few weeks back, when supplies were scarce, the clerk would have a running tally of who’d received a mask, and when. I wash my hands and then I put my n95 on. I need to make sure it’s tightly sealed. It digs painfully into the pressure ulcer on my nose, and my eyes start to water. I practice taking a few breaths — air comes in strained gulps, like I’m sucking it through a straw. That’s good. It’s only safe when it’s difficult to breathe. I put a surgical mask on top, to preserve the n95, and then I clean my goggles again, and put them on. This is the last time I touch my face.
Now I begin cleaning my work station with bleach wipes, to avoid possible contamination from the person who has previously used it. It’s ritualistic and thorough — the same thing, every shift. The first thing I clean is the chair — the back of it, then the seat, then any handles. I move on to the desk — the top and underneath, too. Then my keyboard — between each letter and row. Then I turn it over and clean the back as well. I move on to the mouse, taking care to make sure I also clean the cord and the wheel. The phone is next. I clean again between the numbers and take special care with the receiver. Finally, I wipe down the monitor and any surrounding walls or partitions that I might touch incidentally while working.
I log in and start to review my patient load. Every patient is presumed COVID. A patient with appendicitis? COVID. Stroke? Also COVID. Leg pain? COVID. We’ve learned that every encounter is a potential exposure. So, despite New York being past peak, we can’t afford to be anything less than extremely vigilant.
Before I see my first patient, I wash my hands and put on a fresh pair of gloves. Then I put on a yellow disposable gown over my scrubs, and then a second pair of gloves, making sure that I catch the sleeve of the yellow gown into this second pair, so that my wrists are not exposed. I check my mask and goggles again to make sure they’re snug, and then I go into the room.
. . .
For the next twelve hours, I am home alone with our 21-month-old son, Ronan. I busy myself with my own work while Ronan is napping. When he wakes up, we play and read. I clean the apartment in fits and starts timed to waves of anxiety: I put the toys away, knowing they’ll be pulled out and abandoned again 10 minutes later. I am the Sisyphus of his toy basket. Then, I wipe down commonly touched surfaces, vacuum, and bleach the bathtub where Alex showers.
Around mid-afternoon, I begin dinner and try to make enough for a few meals — I’ve become proficient in lasagnas and stews, anything that reheats well. At 5 PM, I have my third coffee of the day and I put on some music for Ronan. I answer work emails while he dances. I’m engaged with him almost constantly, which makes it difficult to be anywhere but in the present. It’s a blessing that keeps me from worrying about Alex.
At 6:57 PM, our neighbor in the adjacent building exits onto his balcony with his saxophone and plays Take Me Out to the Ball Game, followed by God Bless America. He’s an older gentleman, probably in his early eighties, with a penchant for accessorizing with bright pink — usually a cap, sometimes a cozy-looking cardigan. Ronan bangs on our window and yells “Bavo!” gleefully — he still can’t pronounce his Rs. He’s acknowledged with a wave and a bow from the balcony.
At 7 PM, the cheering starts.
. . .
Once I’m in the room with a patient, I try to maintain a six foot distance. Depending on the situation, I’m usually alone. Sometimes, if the patient is critically ill, there may be a nurse or other staff, but for the most part we try to minimize how many people go in, to conserve PPE. I approach the patient to examine them — I listen to their lungs, I look at the back of their throat, I examine their abdomen for tenderness, and I also look at their legs. We tailor our routine exam for each individual complaint — but these days, the stories all sound similar. A standard history and exam takes about five to ten minutes.
When I’m done seeing the patient, I pull off my yellow gown and, with it, my top layer of gloves. I use the bottom set of gloves to open the door. I close the door shut (or pull the curtain, depending on where the patient is) and take off the remaining pair of gloves. Then, I head to the sink to wash my hands. If the patient was coughing or if I spent a lot of time in close proximity, I usually change the procedure mask and wipe down my goggles. Then, it’s on to the next patient.
Repeat. All day.
I’ve learned that the more I repeat an action or a routine, the better I become at carrying it out successfully and avoiding what we all fear right now, contamination.
It’s OCD-like behavior that I think everyone in the hospital has picked up, to a certain degree, from this pandemic. I don’t deviate from it, at all. I know it’s what keeps me safe.
Stay away from sick people.
She says it to be funny, I think. She knows it’s an impossible ask. But I’m not sure my wife realizes the weight on my shoulders — the responsibility I feel to stay safe. I haven’t hugged my family in over two months — anything to keep them from contracting a virus that could kill them.
And what a way to go.
A patient comes in, DNR/DNI. Brought in by ambulance. Super sick. Blood oxygen level in the 40s. Weak, dehydrated — so dehydrated the nurses can’t get an IV in them. We have to do an IO — intraosseous — drill a needle into their shinbone in order to hydrate and medicate them. It’s a painful procedure but they don’t wince — don’t react to the pain because they’re so sick.
Because of the Do Not Intubate order, there’s not much we can do. A BiPAP machine is briefly an option, but candidates have to be lucid enough to coordinate their breathing with the device. This patient doesn’t have the mental capacity to handle that. We also know that BiPAPs aerosolize the virus — spreading COVID-19 through the air, putting the whole ER at risk.
As I’m discussing the patient’s treatment plan with my team, their partner arrives. They ask to be allowed into the patient’s room because they know what’s coming. They sense it. We all do. The spouse tells me it’s time to stop fighting — to make the patient comfortable. I look into the room — the patient is breathing really fast, clearly in distress, so we give them a little morphine to help ease their breathing.
I huddle with my team and we decide that as long as the partner understands the risk of being in the room, they should be allowed inside. We gown them up, explain safety procedures, and let them in. They sit by the bed and wait, and we watch from the window.
We watch the patient’s blood oxygen numbers plummet, aware of what will happen — any second now. Their partner sits by them and we watch their lips move — we can’t make out any words, just a gentle and soothing murmur.
And then the monitor flatlines.
The alarm blares in the room and throughout the ER and, within seconds, one of our nurses goes in to turn it off. I am on her heels — re-gowned, to call the time of death.
I hold the partner’s gloved hand as they cry inconsolably. Unimaginable: the grief one must feel as they sit helplessly by, watching their loved one grow paler — watching life slowly leave their body. How unfair it feels to withhold human comfort from them in these circumstances.
I feel my grip relax on their hand and I pull them in for a hug. The nurse in the room with me watches for a beat and then joins me quietly on the other side, interlocking her arms around the grieving — a temporary shield.
. . .
“Let’s cheer for papa!” I hand Ronan a stainless steel lid from one of our smaller pots and a wooden spoon, and we march around our small kitchen, making quite the racket.
I wonder, in a brief moment of panic, if and how he’ll remember this when he’s older.
By 7:30 PM, Ronan has had dinner and bathed. We FaceTime with both sets of grandparents, read one last book and at 7:45, he’s in bed for the night.
At around 8 PM, I get a text from Alex: “Done. Coming home.”
This half an hour of solitude is the hardest part of my day. All the fears and anxieties I’ve been warding off finally have a chance to declare themselves, and they do. Greedily, with vengeance — What if today is the day Alex contracted the virus? What if he gets very ill? What if I get very ill? Who will take care of Ronan?
This, followed by some painfully morbid mental accounting: It’s probably better if I die. Alex is stronger than I am. He’ll be able to rebuild. He’ll give Ronan a happier childhood.
I indulge myself in this doomsday thinking because it’s priming my brain for the worst case scenario. If one of us does get sick, it won’t come as a total shock — it won’t totally debilitate me. At least that’s what I tell myself. I need to think about these things and I can’t tell anyone else about them because — well, who would want to spend that time with me, underwater? I feel as if I’ve been bracing for a hit for months now. I’m exhausted.
All Alex and I do is talk about coronavirus. And in spite of all our discussions about numbers, trends, patients, death toll, and vaccines, we seldom talk about what he sees at the hospital. And we never talk about the really scary things, afraid that by breathing them aloud we might call their attention to us.
When did we become like this? Superstitious. Afraid. Illogical.
When Alex finally gets home, he takes his scrubs off outside our front door and stuffs them into a plastic bag that he ties off tightly. He takes his hospital clogs off and leaves them outside, along with his backpack and coat.
We asked our next door neighbor, a lovely 60-something-year-old woman who is battling cancer, if this was alright with her. “Of course, of course,” she said, her eyes filling with tears when we explained that we were afraid Ronan would touch them unwittingly. He gets into everything these days.
Once inside, Alex greets me briefly and jumps into the shower where he spends a good fifteen minutes decompressing and sanitizing himself. I wait for him quietly in the bathroom doorway and listen. Nothing — no loofah scrubbing, no water splashing, and no raspberries from almost-empty shampoo bottles. He’s standing still in the tub, exhausted. I wonder what he’s thinking.
“How was your day?” I ask tentatively.
He says something vague. Okay. Or fine. Or, oh, you know.
I don’t usually push. Some days, vague is what I need. He seems to instinctively sense that.
But something is different now. I am tired of talking around this thing. I am tired of being brave. I am tired of pretending that I don’t want to ask him to quit. Just don’t go in. Stay here with us, stay safe. I have thought it a million times and yet, I can’t bring myself to give voice to it. I just want to hold on to him, even if it’s selfish.
. . .
“It was okay…not that many sick people today.”
She can sense when I’m lying to her, but she needs me to tell her everything is okay. So I do.
I close my eyes in the shower and little frames of the day come back. Some details are more vivid than others — some patients stick with you long after they’re gone. It’s hard to know what your brain will latch on to, what will cause you pain down the road.
The way someone’s eyes look at the exact moment that their heart has stopped beating. The sometimes gurgling, sometimes raspy sound someone makes when they can’t breathe. The way that blood pools and stagnates at the back of the body, a latitudinal divide emerging, almost like half of it has been dipped imperfectly in purple dye. Lividity, it’s called.
I try to wash it all away. Death feels too close to the surface, like if I scrub hard enough, I can push back the fear — the rawness, the animalism. I tell myself what I need to hear to make it palatable — they were older, they lived a good life. I forget what I say when the patient is young. I find something to make it less devastating.
This is what I get stuck on: I am one of the last people someone sees before they’re intubated. Many of them have difficulty breathing, but they’re awake. I watch them struggle with the decision: If we don’t intubate, you’ll most likely die. If we do intubate, your chance of survival is only slightly better. Either way, this may be the last time you’re ever lucid. You have to say goodbye, just in case. They grapple with uncertainty. They’re alone. Their eyes widen, fill with tears. What should I do?They want to know. What would you do?
I wish I could say that I remember all of their faces, that I check their charts afterwards to see whatever happened to them — did they make it? But there are too many.
. . .
Out of the shower, armorless, he seems frail. Just human. Has he been eating enough? No, that’s not what I think. I think: Have I been feeding him enough? Because isn’t that what we’re doing here — manning our lookout towers? Effectively dispatching our responsibilities. Am I doing my part? Am I taking care of you well enough? That’s what we do. We take care of each other; we’re sharp, we’re present, we’re on it. The margin for error is zero.
We’re tired.
“What can I do?” I ask him.
He shrugs, still faraway.
. . .
“What can I do?” my wife wants to know. I go in for a hug, but stop myself.
You can find Helena Dea Bala on Twitter or buy her book Craigslist Confessional.
This piece was edited by Paul Smalera.
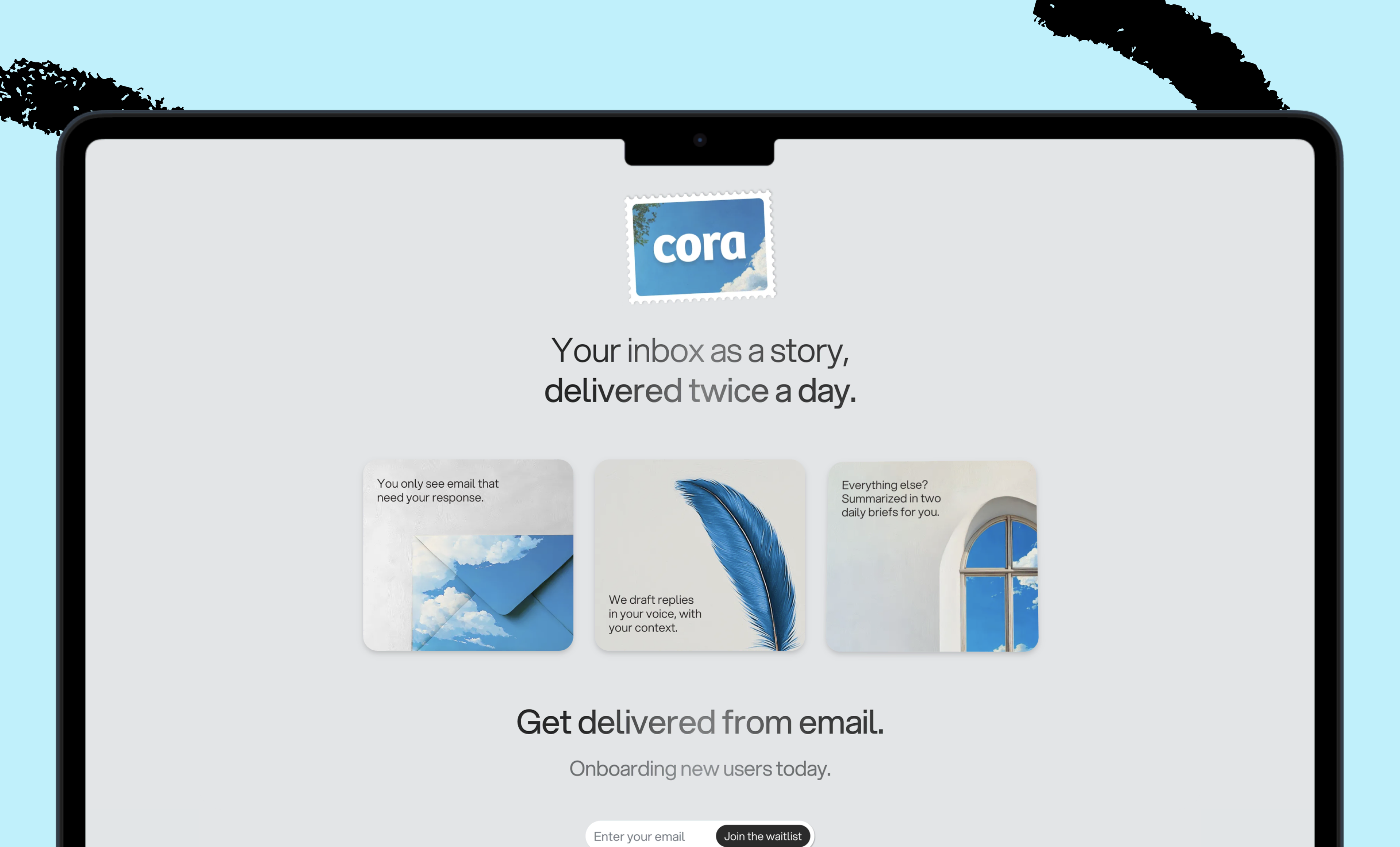
The Only Subscription
You Need to
Stay at the
Edge of AI
The essential toolkit for those shaping the future
"This might be the best value you
can get from an AI subscription."
- Jay S.
Join 100,000+ leaders, builders, and innovators

Email address
Already have an account? Sign in
What is included in a subscription?
Daily insights from AI pioneers + early access to powerful AI tools






Comments
Don't have an account? Sign up!